AESTHETIC PLASTIC
RECONSTRUCTIVE
SURGERY
SEBASTIEN GARSON M.D
BREAST RECONSTRUCTION
This information sheet has been designed under the aegis of Dr DELAY, Emmanuel head of the Plastic and Reconstructive Surgery Department at the Léon Bérard Center, as a complement to your first consultation, to try to answer all the questions you may have if you are considering having recourse to reconstruction. The purpose of this document is to provide you with all the necessary and indispensable information to enable you to make your decision with full knowledge of the facts. You are therefore advised to read it with the utmost care.
Foreword
The information in this booklet is intended to provide you with the key information that can help you decide to have breast reconstruction.
Please remember that the decision for breast reconstruction is a personal choice that you should make after you have been informed and after a period of personal reflection. The spirit of this booklet is to provide you with sincere, clear and honest information, but no document can give you all the answers. Therefore, do not hesitate to ask your surgeon any questions you may have.
Introduction
Every year in France, 42,000 women are diagnosed with breast cancer. Today, however, the physical and psychological consequences are very different from what they were in the past. Advances have been made in the diagnosis, treatment and monitoring of breast cancer patients. Combined with advances in breast reconstruction techniques, they allow patients to benefit from new choices: breast reconstruction is now an option that women can freely discuss with their doctor. The medical profession now recognizes the needs and rights of women to benefit from breast reconstruction after mastectomy. Breasts represent an important part of a woman's femininity, combining her maternal symbolism with her sexual attraction. The significance of the breasts goes beyond purely realistic considerations and the symbolic importance of the breasts persists throughout life.
Almost all women can benefit from breast reconstruction without any limit of age, initial treatment or the number of years that have passed since the removal of the breast. In the case of radiotherapy on the wall, a delay of approximately 1 year is recommended before performing reconstruction (delayed breast reconstruction). In the absence of radiotherapy, reconstruction is possible in the same operative time as breast removal (immediate breast reconstruction).
The goal of a breast reconstruction is to regain symmetry of the breasts when the patient wears a bra or is dressed. The difference between the reconstructed breast and the remaining breast can be noticed when the patient is naked. The final quality of the reconstruction depends very much on the local tissues (skin and muscle) and in particular on the skin tolerance to radiotherapy.
The decision to have a breast reconstruction should be made by a well-informed patient. A wide range of surgical techniques are currently available to offer a solution adapted to each patient. Depending on many factors (patient desires, local tissue condition, tissue that can be removed, general contraindications, cancer status, opposite breast), the plastic surgeon will choose, in agreement with the patient, the most suitable technique among the techniques currently available to reconstruct a breast. During consultations, the presence of a close relative (neutral, caring and loving) is a definite help for the patient.
What is breast reconstruction?
Breast reconstruction is a surgical procedure that, after the removal of a breast, restores the contours of a breast. In a second step, the surgeon will reconstruct the nipple and areola (the brown area around the nipple) and perform, if necessary, a contralateral breast plasty to achieve final symmetry.
There are two main types of procedures: those using a breast prosthesis and those using the patient's own tissue (autologous reconstructions). The choice depends on the quantity and quality of local tissue, the desire to restore the best possible breast symmetry, the history of radiotherapy, and the constraints of the harvesting site. The surgeon and the patient will discuss the best possible choice based on these criteria.
Who can have breast reconstruction?
Breast reconstruction is very often a possibility for women who have had their breasts completely removed. Most patients can benefit from breast reconstruction.
The majority of women choose to wait a certain amount of time after the initial breast removal surgery. Waiting may also be suggested by the surgeon for various reasons: 1 year after the end of radiation therapy; being overweight, high blood pressure or smoking to be corrected before reconstruction. Similarly, if radiotherapy or chemotherapy must be performed soon after the breast removal, the surgeon will prefer to postpone the breast reconstruction. During this waiting period, we advise you to soften the thoracic skin with concentric massages starting from the lower costal area and gradually moving up to the upper parietal area. These maneuvers improve local vascularization and local skin suppleness, thus contributing to better results of the delayed breast reconstruction.
Being informed of the treatment options will allow you to look positively at breast reconstruction and thus your future life.
In delayed reconstructions (one year after radiotherapy), it is desirable that the patient has completed her grieving process before performing the breast reconstruction. The grieving process can be considered well advanced when the patient accepts the idea that she will never regain her breast "as before", nor normal breast sensitivity.
The different breast reconstruction procedures
Techniques using a breast prosthesis
Breast prosthesis only
This is the simplest solution technically. It consists of introducing a prosthesis under the pectoralis major muscle through the mastectomy scar. The shell of this prosthesis is made of silicone and the contents are saline or silicone gel. This technique does not require an additional scar or muscle removal.
Hospitalization is 3 to 4 days. The main disadvantages are:
- The risk of hardening and deformation of the breast (this is the periprosthetic shell).
- A long-lasting breast symmetry rarely obtained (the prosthetic breast does not "age" in the same way as the remaining breast).
- The risk of deflation of the prosthesis (the timing of which is unpredictable) in the case of a saline inflated prosthesis and the risk of siliconoma in the case of a prosthesis pre-filled with silicone gel. It is important to remember that the prostheses have a limited lifespan, which makes it necessary to change them approximately every year (before, if there is a problem; after, if everything is perfect). Currently, we use the silicone gel-filled prostheses that give better morphological results and a more satisfactory consistency than those filled with saline.
Tissue expansion by prosthesis and then definitive prosthesis
It consists of gradually distending the thoracic skin of the pectoralis major muscle by an inflatable prosthesis. The surgeon injects saline through a small valve placed under the skin. The rhythm is usually weekly and lasts two to three months. Then during a second operation, he will replace this inflatable prosthesis with a permanent one. The advantages of this technique are to be able to reconstruct breasts of significant volume and to give the patient the possibility to appreciate the desired volume. The disadvantages are the same as with a prosthesis alone with additional operating time and the constraints related to weekly inflation. Finally, this technique can only be used when the local tissues are of good quality; it is less indicated in the case of chest wall irradiation (radiotherapy), which greatly reduces the indications.
Musculocutaneous flap of large back with prosthesis
When there is poor quality skin tissue or a quantitative skin deficit too great to obtain a satisfactory result with a prosthesis alone, healthy, well-vascularized tissue must be brought in. This technique consists of transferring skin and muscle from the patient's back to the thorax through a subcutaneous tunnel, and placing a prosthesis under the flap to give the desired volume. It is a classic and well codified technique. The disadvantages are those related to the use of a prosthesis, the presence of a dorsal scar and transient dorsal discomfort related to the removal, the difference in skin color and texture giving a "patch" effect, and the frequent occurrence of dorsal seroma (fluid pockets in the back) which may require several punctures during the post-operative period.
Techniques without breast prosthesis: autologous reconstructions
Flap of large backbone without prosthesis
It is a relatively new technique, which is widely used in our team where it has been developed and improved. As in the classic technique of the large dorsal flap, a skin-fat paddle is transposed onto the large dorsal muscle, adding different fat areas of the back that are brought onto the muscle. The volume of the flap is thus considerably increased and makes it possible to do without a prosthesis in about 70% of cases. In the case of delayed reconstruction, we often combine an abdominal advancement flap that allows us to gain volume and create the skin supply that will receive the flap that will give the desired volume. The skin flap can then often be removed and buried, avoiding in this case the patch effect. In the case of immediate reconstruction, it is very often possible to perform a mastectomy with conservation of the skin sheath: the flap is then buried for the most part, with the exception of a round areolar area which will later be used to redo the areolomamelar plate (nipple and areola).
This is a reliable technique that gives a natural consistency and shape to the reconstructed breast. The reconstructed breast integrates well into the woman's body shape. Its disadvantages are: back scarring, post-operative back pain and transient back discomfort, and the frequent occurrence of back seroma (fluid pockets in the back) which often require several punctures during the post-operative period. During the reconstruction time of the nipple-areolar plaque, it is often possible to improve the result by lipomodeling the reconstructed breast. This recent technique, derived from facial cosmetic surgery, has been developed in the department to correct possible imperfections such as a lack of projection, or a lack of volume, or a lack of fullness of the upper part of the breast. This technique consists of taking fat from a donor site (usually the belly or hips), by liposuction with a syringe, centrifuging this fat, and then transferring it to the reconstructed breast, thus improving the result, and often the donor site. The quantity transferred must be hypercorrected in order to obtain the expected result at about 3 months post-operatively. The removal site is the site of bruising and ~edema that takes about 3 months to disappear.
Right rectus abdomen flap (TRAM)
This technique uses the skin-fat paddle under the umbilical cord nourished by the rectus abdominis muscle. The flap is passed under a skin tunnel and then shaped. The abdominal closure is done as in an abdominoplasty (an operation that removes excess skin and fat from the abdomen) and thus creates a lower abdominal scar across the entire width of the abdomen.
The main advantage is that a breast can be reconstructed without the addition of a prosthesis and with a large volume if necessary. The disadvantages are numerous: It is a delicate procedure with a higher blood loss (possibility of autotransfusion), a longer postoperative convalescence than with a reconstruction by large dorsal muscle, a patch effect on the reconstructed breast, a weakening of the abdominal wall with a risk of eventration. Finally, there is a small risk of partial necrosis of the transferred paddle, which may lead to a surgical revision (this risk is greater in smokers, diabetics, and in case of a history of radiotherapy). The ideal indication for this technique is the patient who presents an excess of lower abdominal skin and fat and wishes to correct it with an abdominoplasty.
Microsurgical free flaps
These are mainly the free flaps of the large right abdomen and large lower gluteus. The skin, fat and muscle from these donor sites are removed after cutting the vessels (artery and vein) that nourish them; to keep the tissue alive, the vessels will be reanastomosed (sewn back together) to vessels near the chest using magnifying glasses or an operating microscope. These are very long and delicate operations with important technical constraints (microscope, double team work) and a risk of total necrosis of the flap. The indications for this technique are, in our team, exceptional.
Second operative period
When the reconstructed breast has taken its definitive place, i.e. 4 - 5 months after the first breast reconstruction, a second operation should be performed.
During this time the areola will be reconstructed, the contours of the previously reconstructed breast can be improved and the contralateral breast can be symmetrized.
It is therefore important to know that the contralateral abdomen, hips, breast and nipple may be affected by this second operation.
The nipple will be reconstructed either by removing part of the nipple from the remaining breast, or by removal from another site. The areola will be reconstructed by tattooing. Your surgeon will discuss with you the most appropriate technique for your case. This operation can be done in a delayed manner under local anesthesia, on an outpatient basis, or at the same time as the procedures described below, under general anesthesia.
A symmetrization of the remaining breast may be necessary. This will be performed by a mammoplasty technique which will result in additional scars. These will always be located around the areola, vertically in the lower portion of the breast, and sometimes in the submammary fold horizontally. Your surgeon will also discuss with you the most appropriate technique for your case or whether or not a horizontal scar in the submammary fold is necessary.
Finally, the contours of the breast may be altered. This will be done by liposuction of certain areas and by fat transfer, in order to increase the volume or to fill in certain areas of depression. This fat can be removed from the abdomen or the "saddlebags". These techniques are done at the expense of significant postoperative pain but well relieved by analgesic treatment in most cases. Bruises may persist in the fat removal area for a month, as well as a temporary induration.
At the end of this second operative period and after these various surgical procedures, all the steps of the breast reconstruction are, in most cases, completed. It is important to realize that this will have been achieved thanks to the areas not initially affected (nipple on the contralateral side, breast on the contralateral side and fat on the belly or hips).
Your plastic surgeon
Ask him questions
It is very important that you ask your surgeon any questions you may have. The information in this booklet is not exhaustive. Good information will help you decide whether or not to undergo breast reconstruction. Here is a list of examples of questions we have been asked. You can write others as soon as you think of them.
Examples of questions
Can I benefit from breast reconstruction? What techniques are possible in my specific case? What is the best choice? What is the best choice?
Do you have a lot of experience with this technique?
What result can I expect?
Will the reconstructed breast be very different from the original one?
Will the reconstructed breast be sensitive?
What are the complications I may encounter?
Is the operation painful?
How long will I stay in the hospital?
Will I need a transfusion?
If so, will I be able to donate my own blood?
How long after the operation will I be able to return to normal activity?
How long will I be off work?
When can I resume sports?
Will I be hindered in practicing my sport?
Will I be able to drive my car?
Will it be possible to meet patients who have had this procedure? Will the reconstruction interfere with chemotherapy or radiation therapy? Can the reconstructed breast hide a recurrence of my cancer?
What changes in appearance will the reconstructed breast undergo?
What will happen if I get fat or lose weight?
If I have a prosthesis, will I have to change it and when?
Is the operation covered by social security?
Before your intervention
Planning your surgery you can start talking about breast reconstruction as soon as the diagnosis of breast cancer is mentioned. You will talk to the surgeon who will perform the breast removal so that he or she can contact the plastic surgeon if necessary. Together, they will establish a therapeutic protocol that will allow you to benefit from breast reconstruction in the best possible conditions.
After a clinical examination, the plastic surgeon will explain all the technical possibilities adapted to your case. You will have to discuss your expectations with him. Remember that breast reconstruction after mastectomy can considerably improve your appearance, your well-being and your quality of life. However, it is important to understand that breast reconstruction has its limits and that you will never be able to return to your original breast.
A biological assessment will be performed before your surgery. The consultation with the anesthesiologist will take place during the month prior to the procedure (bring all the particular elements corresponding to your medical or anesthetic history, accompanied by a letter from your attending physician in case of specific problems or treatments).
Advice to be respected
The surgeon will give you specific instructions in order to reduce the risk of operative and postoperative complications. This mainly involves avoiding alcohol, cigarettes (smoking must be stopped 1 month before and 1 month after the operation) and medications that may cause bleeding and bruising (in particular, stop taking aspirin-based medications and anti-inflammatory drugs 15 days before the operation). From the day after the operation, walking is recommended (going to the corridor and walking) because it reduces the risk of phlebitis and shortens the post-operative recovery phase. Depending on the reconstruction technique chosen and on your family environment, you may need help when you return home.
Possible surgical risks
Breast reconstruction, like any surgery under general anesthesia, may expose you to complications such as hemorrhage, hematoma, infection, or complications of anesthesia. Complications of general anesthesia, which are potentially serious, have become exceptional at this time.
Smoking patients have a higher risk of delayed healing, especially if they have had chest wall radiation therapy. The quality of the final scar may then suffer. Sometimes these complications may require a surgical revision.
The risk of infection may occur during the first weeks after surgery. If a breast prosthesis has been placed, it will have to be removed and replaced a few months after healing.
The most common problem encountered after implant placement is the periprosthetic shell. The breast becomes hard and sometimes painful and often requires corrective surgery. Inflatable prostheses expose a risk of deflation that increases with the duration of implantation.
With the technique using the large back flap without prosthesis, the occurrence of a back seroma is the most common problem encountered. This is the creation of a fluid pocket in the back, usually in the lower part of the back. This problem, which is more of an inconvenience than a complication, is very common but without consequence. It will only require one or more back punctures (painless) to dry this seroma.
Finally, the technique using the rectus abdominis muscle (TRAM) involves a higher risk of phlebitis (and therefore pulmonary embolism) because the patient is more embarrassed to walk in the days following the procedure. The risk of necrosis of part of the flap and delayed healing of the abdomen must be taken into account as this may lead to additional surgery. Finally, there is a risk of weakening of the abdominal wall, or even of abdominal venting, which may require corrective intervention at a later date.
After breast reconstruction
What to expect?
The first night is relatively painful, but the prescribed pain medication is usually effective. The painful discomfort persists for 3 or 4 days, then gradually fades away in a variable period of time depending on the patient. You will then be tired after the procedure. This fatigue lasts one to two weeks if only a prosthesis is used, three to four weeks after reconstruction using a flap of the greater backbone, and up to three months after reconstruction using the rectus abdominis muscle (TRAM).
Depending on the type of surgery and your recovery, you will remain hospitalized for 3 to 7 days. Redon drains are used to remove blood and serosities. They are removed as soon as they give few serosities. During a flap reconstruction of a large back without a prosthesis, the patient goes home with a drain located in the back. The drain will be removed after one week (two weeks after surgery) during a post-operative consultation. Dressings will be applied every three days by a home nurse who will also remove the few non-absorbable stitches on the tenth day of the operation. In the case of a flap reconstruction of a large back without prosthesis, a compressive back belt is usually prescribed, which will be worn from the date of the removal of the last drain and for a period of 15 to 20 days, possibly extended in the event of a back seroma.
Return to normal activity
It will take about six weeks to return to normal activity after flap reconstruction, less in the case of a prosthesis alone. The prescribed work stoppage is usually 3 weeks after prosthesis reconstruction, 1.5 months after long back flap, and 3 months after rectus abdominis (TRAM). These durations are indicative; they may be shorter or longer depending on the speed of recovery of patients and their personal and psychological balance.
The morphological and esthetic result of the reconstruction can only be reliably evaluated after a period of 3 to 5 months after reconstruction of the areolomamelonal plate with possible symmetrization of the contralateral breast.
The sensitivity of the breast is not directly restored by the procedure. Nevertheless, after reconstruction with autologous tissue, sensitivity gradually reappears after several months and progresses over a period of approximately two years.
Sensitivity disorders (inner arm) and possible shoulder disorders, related to axillary healing, are not modified by the breast reconstruction procedure.
The scars will fade after one year but will never disappear.
Ask your surgeon for advice, but sports and sexual activity should be avoided for the first month. Swimming is the most recommended sports activity after breast reconstruction, especially after flap reconstruction without prosthesis; it is the fastest way to recover the shoulder and back without the risk of pain.
Finally, it is important to know that it takes time to get used to the reconstructed breast and that there is often a period of ambivalence ("did I do well to be reconstructed?") of 6 to 7 months, explaining that full satisfaction with the procedure only comes after this period, which can be longer or shorter depending on the patient. The medical, family and friendly, caring environment plays an important role during this period when the patient needs reassurance. Talking with other women who have benefited from this procedure previously, or with a psychologist, can help the patient express and manage her emotions. It is also important to be aware that the reconstructive procedure may reactivate psychological difficulties that the woman had experienced during the mastectomy; it is important not to feel guilty about this, but rather to express them (with or without the help of a psychologist) as this is an opportunity to manage them more positively.
Is there a risk of cancer recurrence after reconstruction?
Breast reconstruction is not a factor in breast cancer recurrence.
It does not promote or prevent recurrence. Moreover, it does not interfere with possible chemotherapy or radiotherapy in case of recurrence. It does not usually interfere with post-treatment monitoring. In some rare cases, it allows the diagnosis of recurrence or the diagnosis of occult breast cancer of the contralateral breast (in the case of a possible symmetrization breast plasty).
Conclusion
After the period of normal post-operative constraints, breast reconstruction brings a lot to patients in terms of rehabilitation, well-being and quality of life.
Breast reconstruction is not an urgent intervention.
It should be considered more as a possibility and a positive choice (which you may decide to do), than as an obligation (which you would undergo).
You must take your time to make the best choice.
The consultation with the plastic surgeon is the most important step to give you all the necessary information.
You should not hesitate to review it, even several times if necessary, before making your decision.
CONTACT
Contact Us
Phone : + 33344282959
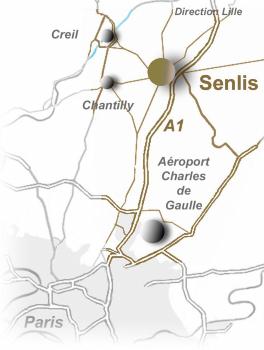
Address:
7 impasse de la Passerelle 60300 SENLIS
France
Copyright SELARL Dr Garson Pages d'information- Crédits photos : Dr Garson / Libre de droits - Mentions légales
Ce site utilise des cookies à des fins statistiques - Pour en savoir plus, cliquez ICI.
SITE RÉALISÉ AVEC WEBACAPPELLA RESPONSIVE